With Mississippi Coast temperatures hovering in the mid-to-high 90s, coupled with the high humidity, the heat index often tops 105 degrees this time of year. These conditions can be deadly for those who don’t have access to adequate fluids and cooled environments. The devastating health emergencies extreme heat can trigger include kidney shut down, stroke, and cardiac arrest.
Certain individuals are at especially high risk. Disabled people who rely on others to bring them fluids may not be able to respond to their own needs. Many homeless live in their cars, and a dark-colored vehicle parked in the sun can reach an interior temperature of 200 degrees quickly. Young children have increased susceptibility to heat illnesses, both because they’re unable to voice their need for fluid and their smaller body mass gives them much less reserve to tolerate fluid loss.
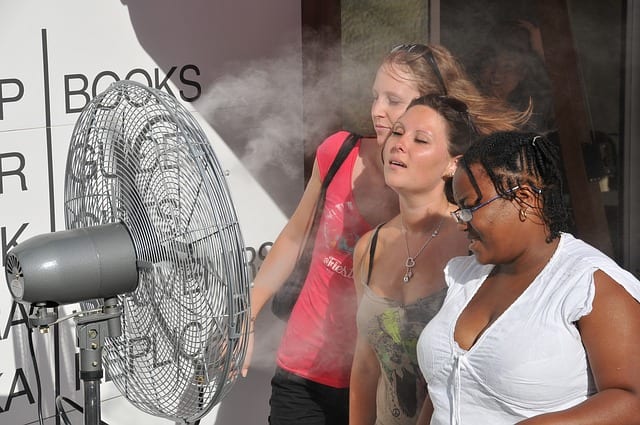
I remember one case in which a mother left her child in the car seat with the windows cracked. The toddler was sleeping, and the mother was just running into the store for a moment. The checkout line was longer than she had anticipated, and by the time she came back and checked on the baby, she couldn’t wake him. Fortunately, she recognized the danger and rushed him to our ER, where we immediately administered IV fluids and used evaporation fans. The child had a four-day hospitalization before recovering.
Heat illnesses range from mild, such as rash, swelling or fainting, to the potentially deadly heatstroke. One of the earlier stages is heat exhaustion. Someone who is affected will sweat profusely and show a weak pulse, and they also can become nauseated and confused. One elderly woman I treated had her electricity cut off because she couldn’t afford the payments. She had been vomiting for three days with resultant electrolyte loss, and it took over six liters of IV fluids before her kidneys started working again. The elderly are particularly vulnerable to heat illnesses because they often lose their ability to self-regulate their body temperature, known as loss of thermoregulation, and they also have a decreased sense of thirst.
In over 40 years of being an ER doctor in the South, I’ve seen the worst stage of heat illness, heat stroke, only a few times. The body loses the ability to cool itself, with the victim having headaches, flushed skin, racing pulse, and elevated temperatures — typically over 105. I remember one time the rescue squad brought in an alcoholic man who’d been living in a makeshift tent he’d set up in the woods. With too much heat and too little water, he had passed out. By the time the patient arrived in the ER, he was having seizures. Despite our efforts; fluids, dialysis, and cooling methods, he succumbed to his multi-system failure, dying within 24 hours. Intoxicants and some drugs increase the effects of heat illness. Not only do they impair a person’s judgment, but alcohol and medications can interfere with the body’s normal abilities to cope with the heat by disrupting sweating and kidney functions.
Now in the hottest days of our Mississippi summer, be aware of the dangers of excessive heat. This illness is made worse by the accumulation of overheating and dehydration over several days but can occur in a matter of a few hours. Check on your neighbors, particularly those without air conditioning and those living without shelter. Your concern for those in need may be lifesaving.
Image by Selcuk YILDIZ from Pixabay
Dr. Philip L. Levin is based in Gulfport and has been practicing medicine for 40 years. He graduated from the University of Texas Medical School at San Antonio in 1978 and specializes in emergency medicine. He can be contacted at (228) 867-4000.